Medically-Boosted Placebo Effect May Help Some Chronic Patients
May 19, 2021
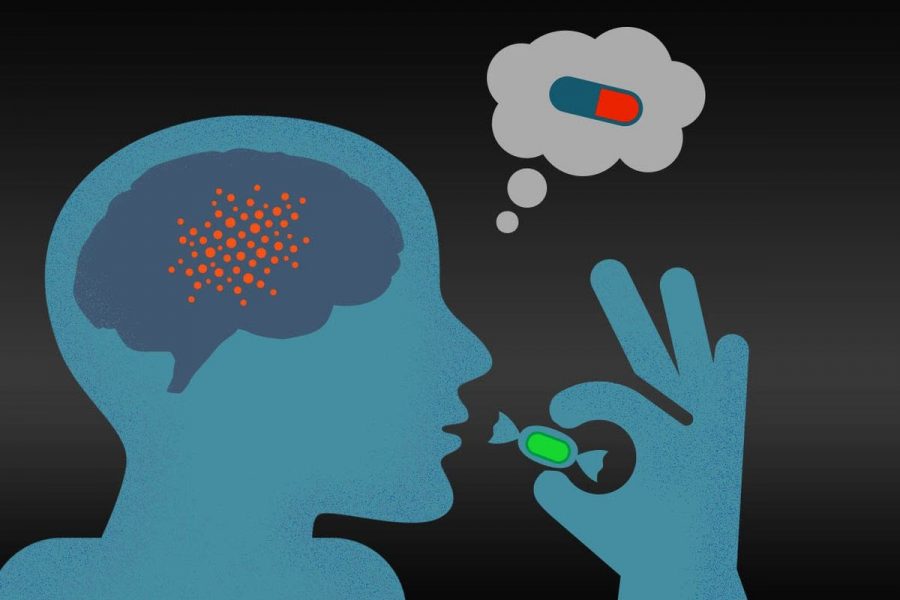
In a recent study, scientists have been able to begin to harness the intricate power of the placebo effect on the human brain. On May 3rd, scientists reported their findings from the study online in Proceedings of the National Academy of Sciences. What they found raises the possibility of enhancing the power of expectations to improve treatments for a range of conditions, including those involving chronic pain.
The placebo effect is the positive effect on a person’s health experienced after taking a placebo. This could be an inactive substance, like a sugar pill. It is triggered by the person’s belief in the benefit from the treatment and their expectation of feeling better, not the characteristics of the placebo. These effects can be boosted by electrical currents which means that this technique could benefit some, but not all chronic patients, given that chronic pain presents itself differently in everyone and isn’t always caused by injury.
This is the first study that has been able to prove that placebo and blunt pain-inducing nocebo effects can be boosted by altering brain activity. The nocebo effect is the placebo’s evil twin: A person feels worse after taking an inactive substance that they expect to have unpleasant effects.
To play with people’s expectations, Dr. Kong’s team primed 81 participants for painful heat. The heat was delivered by a thermal stimulator to the forearm while participants lay in a functional MRI scanner. Each person received three creams, each to a different spot on their arms. One cream, participants were told, was a numbing lidocaine cream, one was a regular cream and one was a pain-increasing capsaicin cream. But in fact, all the creams were the same inert lotion, dyed different colors.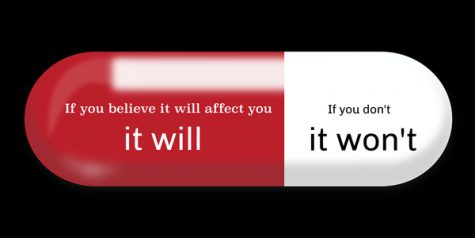
Before testing the effects of placebo and nocebo effects, the researchers had delivered electric currents to some participant’s brains with a method called trans-cranial direct current stimulation AKA tDCS. During the tDCS sessions, two electrodes were attached to the scalp and delivered a weak electric current into the brain, allowing for the change of neuron behavior.
Participants who received “lidocaine” reported lower pain intensity from the heat stimulator, proving the placebo effect, while those who received “capsaicin” rep0rted a higher pain intensity, an expected nocebo effect.
Some participants received tDCS targeted at a brain area thought to be important in placebo and nocebo effects, the right dorsolateral prefrontal cortex. Researchers used two types of current: positive anodal tDCS, which typically makes nerve cells more likely to fire off signals, and negative cathodal tDCS, which usually makes cells quieter. Compared with people who didn’t receive tDCS, people who received cathodal tDCS reported stronger placebo effects when heat was applied to the skin with “lidocaine” cream. For people who received anodal tDCS, the stimulation dampened the nocebo effect of the “capsaicin” cream which was a groundbreaking discovery in this study.
This is only the beginning of being able to harness the placebo and nocebo effects in order to control chronic pain, but the results from this study have spoken for themselves. The research team plans on attempting to replicate these results in chronic pain patients as it’s a widespread issue within America with 20% of adults reporting pain lasting more than six months in just 2016, we can only imagine how much that number has grown since then.
This is one of the first studies of its kind, but another study done in September of 2018 has shown that there are certain neurobiological and personality characteristics that have been found to make humans more susceptible to placebo treatment. By analyzing the brain images, the team found that these patients, compared with people who weren’t susceptible to the placebo, had a difference in volume between the right and left sides of the limbic system in the brain, which is involved in instinct and mood. There were also differences in the number of nerve cell connections between the prefrontal cortex and other brain areas. Personality questionnaires revealed that these people had a higher self-awareness and openness than nonresponders.
“It is surprising and encouraging that it may be possible to predict the magnitude of a placebo effect before treatment,” says Tor Wager, a neuroscientist at the University of Colorado Boulder, who was not involved in the research. More work is needed to see how the predictive features hold up in other populations and for different pain conditions.